| CATEGORII DOCUMENTE |
| Bulgara | Ceha slovaca | Croata | Engleza | Estona | Finlandeza | Franceza |
| Germana | Italiana | Letona | Lituaniana | Maghiara | Olandeza | Poloneza |
| Sarba | Slovena | Spaniola | Suedeza | Turca | Ucraineana |
Although not as common as femoral shaft or hip fractures, fractures of the distal femur present considerable challenges in management. Severe soft-tissue damage, comminution, fracture extension into the knee joint, and injury to the quadriceps mechanism lead to unsatisfactory results in many cases, regardless of the treatment. No single method of management has overcome all of the problems associated with these fractures. Before 1970, the majority of supracondylar fractures were treated nonoperatively. However, difficulties were often encountered, including persistent angulatory deformity, knee joint incongruity, loss of knee motion, and delayed mobilization (especially in patients with multiple injuries).217,224,244
During the past two decades, as technology and implants have improved, most traumatologists have advocated some form of internal fixation in the management of distal femoral fractures.206,207,210,214,215,216,217,221,222,223,225,232,237,238,239,241,243,244,248,249,250,251,252,256,258,260,261,262 However, osteosynthesis of the supracondylar region of the femur can be difficult for several reasons. Thin cortices, comminution, osteopenia, and a wide medullary canal make secure internal fixation difficult to achieve, even for an experienced surgeon. Although better methods of fixation have improved clinical results, the operative management of these difficult fractures is far from uniformly successful.226
ANATOMY AND MECHANISM OF INJURY
The shaft of the femur is nearly cylindrical, but at its lower end it broadens into two curved condyles. Anteriorly, the articular surfaces of the two condyles come together to form a surface for articulation with the patella. Posteriorly, they are separated by a deep intercondylar fossa that gives attachment to the cruciate ligaments of the knee. The contact surface for the patella includes parts of both condyles but is derived predominantly from the lateral condyle. The lateral condyle is broader and extends farther proximally. An epicondyle arising from its lateral surface gives rise to the fibular collateral ligament. Immediately below the lateral epicondyle is an oblique groove that houses the tendon of the popliteus tendon.
The medial condyle is longer than the lateral condyle and extends farther inferiorly. Its medial surface is convex and contains an epicondyle that gives attachment to the tibial collateral ligament. Situated on the uppermost part of the condyle is the adductor tubercle on which the tendon of the adductor magnus muscle inserts.
The expanded femoral and corresponding tibial condyles are adapted for the direct downward transmission of weight. During weight bearing, the two condyles rest on the horizontal plane of the tibial condyles and the shaft of the femur inclines downward and inward. This inclination is an expression of the greater width of the body at the hips than the knees.
The supracondylar area of the femur is defined as the zone between the femoral condyles and the junction of the metaphysis with the femoral shaft. This comprises the distal 9 cm of the femur, as measured from the articular surface. It is important to distinguish supracondylar fractures from low diaphyseal fractures of the distal femur because the methods of treatment and prognosis are considerably different.
The mechanism of injury in most supracondylar fractures is thought to be axial loading with varus/valgus or rotational forces. In younger patients, the injury typically occurs after high-energy trauma related to motor vehicle or motorcycle accidents. In such patients there may be considerable fracture displacement, comminution, open wounds, and associated injuries. In elderly patients, fractures frequently occur after a minor slip and fall on a flexed knee, leading to comminuted fractures through compromised osteoporotic bone.
The deformities that result from supracondylar femoral fractures are produced primarily by the direction of the initial fracture displacement and secondarily by the pull of the thigh muscles. Spasm and irritability in the quadriceps and hamstrings usually lead to limb shortening and angulation at the fracture site. The typical varus deformity is usually the result of the strong pull of the adductor muscles. Contraction of the gastrocnemius muscle often produces posterior angulation or displacement of the distal fragment. In fractures with intracondylar extension, muscle attachments to the respective femoral condyles tend to produce splaying and rotational malalignment and contribute to joint incongruity. Anterior displacement or angulation seldom occurs in supracondylar fractures.
CLASSIFICATION
There is no universally accepted method of classification for supracondylar fractures of the femur. Essentially all classifications distinguish between extraarticular, intra-articular, and isolated condylar lesions. Fractures are further subdivided according to the degree and direction of displacement, the amount of comminution, and the involvement of the joint surfaces. Unfortunately, anatomical fracture classifications fail to address the conditions commonly associated with supracondylar femur fractures, which often influence treatment or outcome. These factors, which play a dynamic role in management, determine the 'personality' of a fracture. Among these are (1) amount of fracture displacement, (2) degree of comminution, (3) extent of soft-tissue injury, (4) associated neurovascular injuries, (5) magnitude of joint involvement, (6) degree of osteoporosis, (7) presence of multiple trauma, and (8) complex ipsilateral injuries (ie, patella or plateau fracture).221,222,231,245
Many classification systems have been used for fractures of the distal femur, including those of Neer and associates Stewart and coworkers,254 Schatzker and Tile,245 Seinsheimer,246 and Mller and colleagues.235 Neer and associates,236 in 1967, developed a classification based on the direction of displacement of the distal fragment. They hoped this would identify the mechanism of injury and soft-tissue patterns and would ultimately influence treatment. In this classification, four anatomical patterns were recognized. Unfortunately, the Neer classification is based on the relationship of the condyles to the proximal fragment and does not take into account associated intra-articular fractures or joint incongruity. Seinsheimer246 developed his own classification for fractures of the distal femur, which addressed the problems of articular disruption. In this system, fractures are divided into four basic groups, with several subtypes. Although cumbersome, this classification allows the surgeon to analyze results based on a specific fracture group or subtype. Mller and colleagues in what is probably the most widely accepted classification of supracondylar fractures, identify three general types, each with three subtypes, based on radiographic appearances (Fig. 28-44). Because of the large number of fracture patterns seen in clinical practice, it is obvious that some fractures do not fit neatly into any classification scheme. This emphasizes the fact that every case must be individually evaluated, and the 'personality' of the fracture must be considered in selecting the method of treatment.
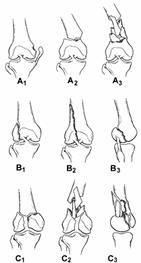
Fig. 28-44
METHODS OF TREATMENT
Considerable controversy exists as to whether nonoperative or surgical treatment leads to the best results for management of supracondylar femoral fractures. Early attempts at internal fixation of these complex injuries were associated with high incidences of malunion, nonunion, and infection. Because of the increased risk of complications, numerous authors concluded that closed methods were preferable to operative treatment.211,212,233,236,254 Stewart and coworkers popularized the two-pin method of skeletal traction, which permitted some knee motion while the patient was in traction.254 However, displaced intra-articular fractures defied such closed methods. Neer and associates236 reviewed a large series of supracondylar fractures and reported good results in 84% of patients treated by closed methods but only 54% good results in surgically treated patients. Although nonoperative therapy generally yielded good results, Neer and associates pointed out several pitfalls with the use of traction therapy. These include excessive knee flexion, varus and internal rotation deformity, inadequate traction x-rays, and overimmobilization of the knee joint.
Traditionally, nonoperative management has included a closed reduction of the fracture, prolonged skeletal traction, and cast immobilization. This method requires confinement to bed, is time consuming and expensive, and is not well suited for patients with multiple injuries or for elderly patients. Although the risks of surgery are avoided with closed methods, malalignment and knee stiffness are commonly encountered. Some of the problems of prolonged traction treatment of supracondylar fractures can be circumvented by using ambulatory cast-brace methods. Numerous authors have shown shorter hospital stays, earlier ambulation and weight bearing, better knee motion, and decreased incidences of nonunion with this treatment approach.211 It must be kept in mind, however, that early reports comparing nonoperative to operative therapy predate both modern internal fracture fixation methods and cast bracing.224
There are several indications for nonoperative treatment of supracondylar femur fractures. Most are limited to fractures without joint involvement. Relative indications for nonoperative therapy include (1) nondisplaced or incomplete fractures, (2) impacted stable fractures in elderly osteoporotic patients, (3) lack of modern internal fixation devices, (4) unfamiliarity or inexperience with surgical techniques, (5) significant underlying medical diseases (eg, cardiovascular, pulmonary, neurologic), (6) advanced osteoporosis, (7) spinal cord injury with fracture, (8) severely contaminated open fractures (type IIIB), (9) selected gunshot wounds, and (10) infected fractures.
Closed fracture management should only be considered if skeletal traction is used in conjunction with early cast-brace techniques. Exceptions to this are nondisplaced fractures and impacted, well-aligned fractures in elderly patients who can be splinted or casted directly. Most fractures can be reduced by traction through a distal femoral or proximal tibial pin. However, placement of a distal femoral pin can be difficult because of significant soft-tissue swelling, hemarthrosis, and fracture comminution. If nonoperative therapy is chosen, insertion of a femoral traction pin under fluoroscopy in a radiology suite or operating room should be considered. Alternatively, longitudinal tibial pin traction with a second vertical force applied through a distal femoral pin may improve the quality of reduction.254 Isolated tibial pin traction is reserved for patients in whom planned internal fixation is delayed more than 8 hours. Twenty to 30 pounds of traction is required to reduce supracondylar fractures in adults. Once length and alignment are restored, this weight can often be decreased. Traction is instituted with a Thomas splint and Pearson knee attachment. Conversion to Neufeld rolling traction should be considered if the duration of traction will exceed 2 or 3 weeks.208
The goal of nonsurgical treatment is not anatomical reduction of the fracture fragments but restoration of overall length and axial alignment. Because of the proximity of the fracture to the knee joint, small degrees of malalignment may have adverse long-term effects on the joint mechanics. Although treatment must be individualized for each patient, no more than 7 of malalignment in the frontal plane (mediolateral) should be willingly accepted. Whenever possible, malalignment in the sagittal plane (anteroposterior) should not exceed 7 to 10. Limb shortening of 1 to 1.5 cm usually does not compromise the functional result. Except in unusual circumstances, articular incongruity of more than 2 mm should not be tolerated. While in traction, patients should be encouraged to attempt limited knee flexion. When the acute soft-tissue swelling has subsided, there is minimal tenderness at the fracture site, and x-rays show early callus formation, the patient can be transferred to a fracture brace. This can be made from plaster, fiberglass, or polyethylene and should allow full knee motion. A fracture brace should be placed between 3 and 6 weeks after injury, correlating clinical signs with symptoms and radiographic evidence of callus formation. It should be applied with the limb in extension, external rotation, and slight valgus. A quadrilateral socket is recommended but not absolutely essential. In this position, varus, the most frequent postcasting complication, is minimized. Another common error is failure to include the entire fracture within the fracture brace. Application of a fracture brace should not lull the surgeon into a false sense of security. Careful attention to the details of fracture reduction and the mechanics of cast-brace application are crucial to the success of the procedure. Clinical and radiographic follow-up at 1, 2, and 3 weeks after cast-brace application is necessary to guard against unrecognized loss of reduction. The brace is worn until the fracture is healed, which is usually by the end of the fourth month.
Occasionally, fracture brace techniques are used in conjunction with limited internal fixation. In comminuted supracondylar femur fractures with nondisplaced or minimally displaced articular extensions, percutaneous cannulated screws can be inserted across the femoral condyles to stabilize the joint. Patients can then be treated with tibial pin traction and subsequent fracture brace techniques.
Operative Treatment
In the past 25 years internal fixation of displaced supracondylar femoral fractures has gained widespread acceptance as operative techniques and implants have improved. The combination of properly designed implants, a better understanding of soft-tissue handling, perioperative antibiotics, and improved anesthetic methods have made internal fixation safe and practical.219,221,222,229,231,239,241,243,250,251 Since 1970, essentially all studies comparing the results of operative and nonoperative methods have favored operative stabilization of supracondylar fractures. Schatzker and associates243 reviewed 68 supracondylar fractures of the femur treated over 6 years. They found that 75% of fractures stabilized with an AO blade plate had excellent to good results. However, only 32% of patients treated nonoperatively had good or excellent results. In a follow-up study, Schatzker and Lambert244 showed that when rigid internal fixation was achieved, 71% of patients had excellent or good results. In contrast, when stable fixation was not achieved or bone graft was not performed, only 21% had excellent or good results. Mize and colleagues232 stressed that in complex intra-articular fractures an extensile exposure with osteotomy of the tibial tubercle greatly facilitates reduction and fixation. This is particularly useful if the medial femoral condyle is comminuted, internal fixation has been delayed more than 10 to 14 days, or the patient has an ipsilateral depressed tibial plateau fracture requiring repair (Fig. 28-45).
The goals of operative treatment of supracondylar femoral fractures are anatomical alignment, stable internal fixation, rapid mobilization, and early functional rehabilitation of the knee. Internal fixation of these injuries is difficult. Fixation unquestionably produces the greatest chance for an excellent result, but complications after its use can also produce the poorest results. Incorrectly performed osteosynthesis is almost always worse than nonoperative treatment (Fig. 28-46).
The operative techniques are complex, and it is essential to have complete sets of instruments and implants available, as well as experienced surgical, nursing, and physiotherapy staff. If these criteria are met, there are several strong indications for operative treatment:
Displaced intra-articular fractures
Patients with multiple injuries (to permit early mobilization)
Most open fractures
Associated vascular injuries requiring repair
Severe ipsilateral limb injuries (ie, patellar fractures, tibial plateau fractures)
Major associated knee ligament injuries
Irreducible fractures
Pathologic fractures

Fig. 28-46 Fractura iatrogena a portiunii posterioare a condilului femoral secundara plasarii intraarticulare a lamei-placii. Malreducere in varus a fracturii.
Relative indications for internal fixation include the following:
Displaced extra-articular supracondylar femoral fractures
Marked obesity
Advanced age
Fracture around a total-knee replacement
Contraindications to fracture fixation include
Active infection
Severely contaminated open fractures (type IIIB) (acutely)
Massive comminution or bone loss
Severe osteopenia
Patients with unstable multiple injuries
Inadequate facilities
Inexperienced surgeons
In isolated closed, displaced supracondylar fractures that require surgery, internal fixation should be performed within the first 48 hours. If surgery is delayed for more than 8 hours, the patient should be placed in tibial pin traction. Closed fractures in patients with multiple injuries should be stabilized during or at the conclusion of thoracic, abdominal, vascular, or neurosurgical procedures whenever possible.
Open fractures constitute 5% to 10% of all supracondylar femoral fractures. The traumatic wound is nearly always anterior and is associated with a variable degree of damage to the extensor mechanism. As with all open fractures, urgent but thoughtful treatment is required. Thorough irrigation and debridement of the fracture and traumatic wounds remains the single most important step in the prevention of infection. Serial debridement may be necessary in many type III open fractures. With few exceptions (eg, coverage of an exposed joint), the traumatic wound should be left open. If immediate internal fixation of the open fracture is performed, the surgical extensions can be closed, but the open fracture wounds should not be closed primarily. Immediate internal fixation is not indicated for all fracture patterns. The risk-benefit ratio to the patient must be carefully assessed when contemplating primary internal fixation. Internal fixation for open fractures is particularly useful in patients with multiple injuries, massive and mutilating limb injuries, open fractures with vascular injuries, and open intra-articular fractures. Advantages of immediate internal fixation in these fractures include stabilization of the fracture and surrounding soft tissues, ease of wound care, pain relief, and mobilization of the patient and the injured limb. The major disadvantage of immediate internal fixation in open supracondylar fractures is the increased risk of infection as a consequence of further soft-tissue dissection and interference with local blood supply. If infection develops, it may affect not only the fracture site but also the knee joint.
In patients with type I, II, and IIIA open supracondylar fractures, experienced fracture surgeons favor definitive internal fixation after debridement of the traumatic wounds (Fig. 28-47). However, most grade IIIB and IIIC open supracondylar fractures are more safely managed with external fixation across the knee or with skeletal traction and delayed internal fixation. For less experienced fracture surgeons, delayed internal fixation of all open supracondylar fractures may be advisable. After irrigation and debridement of the wounds, the injured limb can be splinted or placed in skeletal traction. Subsequent surgery can be carefully planned with optimal operating room personnel. Unfortunately, many open supracondylar fractures occur in patients with multiple injuries, and failure to stabilize the fracture acutely often leads to missed opportunities. Associated injuries and pulmonary problems may delay the definitive fixation for days or weeks. This delay increases the technical difficult of the procedure, contributes to patient morbidity, and compromises the full benefits of internal fixation.
The exact incidence of vascular injury accompanying supracondylar femur fracture is unknown but is estimated to be only 2% to 3%. Most injuries to the superficial or profunda femoral arteries occur after fractures of the femoral shaft. On the other hand, blunt injury to the popliteal artery most commonly accompanies dislocations of the knee or displaced fractures of the proximal tibia. It is surprising, therefore, that the incidence of popliteal artery injury is so low after supracondylar fracture, because the vascular bundle is tethered proximally in the hiatus of the adductor magnus muscle and distally by the arch of the soleus. These tight attachments leave little room for skeletal distortion after fracture. Vessel injury can be caused by direct laceration or contusion of the artery or vein by fracture fragments or indirectly by stretching leading to intimal damage. Clinical examination of the leg for signs of ischemia with evaluation of pulses and motor and sensory function is essential.
Indications for arteriography include an absent or diminished pulse, expanding hematoma, bruit, progressive swelling, persistent arterial bleeding, and injury to anatomically related nerves. Displaced supracondylar fractures in close proximity to the femoral or popliteal vessels despite apparent normal peripheral pulses may have occult vascular injury patterns and require careful judgment regarding the need for exploration or angiography. If any doubt exists about the integrity of the vessels, it is wise to proceed with an angiogram to rule out an occult vascular injury. Doppler ultrasound cannot rule out an intimal tear and is not recommended.
The treatment of arterial injury in conjunction with supracondylar femur fractures depends on the severity of the ischemia and amount of time elapsed since the injury. If distal pulses are present (indicating distal tissue perfusion), the fracture should be fixed first. If arterial compromise is severe or the time elapsed from injury is more than 6 hours, reestablishment of circulation takes priority. This can be achieved either by temporarily shunting the arterial flow or by definitive vascular repair. Arterial repairs are usually accomplished by interposition vein grafts or synthetic grafts. Whenever possible, concomitant femoral or popliteal vein injuries should be repaired. One of the most common and preventable mistakes is to repair the vessel with the fracture in a displaced position. During subsequent fixation of the fracture, manipulation of overriding fragments can disrupt the anastomosis. This problem can be avoided or minimized by using a temporary external fixator or a femoral distractor to maintain length and alignment during the vascular repair. Fasciotomy of the lower leg should be considered in all patients with ischemia time exceeding 6 hours who have tenseness of the fascial compartments after reperfusion or extensive soft-tissue injuries. Compartment pressure monitoring may be helpful.
In patients with massive open wounds with vascular injury (type IIIC), primary amputation may be indicated. This is particularly true if the injury is associated with sciatic or posterior tibial nerve deficits. The goal of aggressive limb salvage should be functional viability, not just a perfused limb.
Modern concepts in the surgical management of supracondylar femoral fractures were provided by the Association for the Study of Internal Fixation (ASIF) in Switzerland.235 A key component in the Swiss philosophy of fracture care is detailed preoperative planning.229,245 The surgeon, through a set of preoperative drawings, can deduce the best method of solving a difficult problem. The surgery is performed on paper before being carried out in the operating room. Executed properly, this surgical tactic shortens operative time, minimizes intraoperative decision making, and improves results. In preoperative planning for a supracondylar femoral fracture, high-quality x-rays of both the intact femur and the injured side are necessary. With the use of plastic templates, the fracture and its subsequent reduction, together with the type and size of implants and the exact position of screws, can be sketched on tracing paper. Multiple drawings are frequently necessary to arrive at the optimal fixation construct with the least soft-tissue dissection. Careful preoperative planning often clarifies the need for supplemental bone grafts. More importantly, it ensures that proper implants are available at the time of surgery. The sequential steps in the surgical management of supracondylar femoral fractures include (1) restoration of the articular surface, (2) stable internal fixation, (3) bone grafting of comminuted metaphyseal segments, (4) impaction of the fracture in osteoporotic elderly patients, (5) repair of associated ligament injuries and patellar fractures, (6) early range of motion of the knee, and (7) delayed, protected weight bearing.251,262
Patients should be positioned supine on a radiolucent table with the ipsilateral hip elevated to allow slight internal rotation of the leg. An image intensifier is strongly recommended. The entire leg and ipsilateral iliac crest are prepped and draped into the operative field. In many cases a sterile tourniquet can be used for part or all of the case. In most patients, surgery can be performed through a single long, lateral incision. In supracondylar fractures with intra-articular involvement, the incision should extend across the knee joint ending distal and lateral to the tibial tubercle. The incision remains anterior to the lateral collateral ligament. The vastus lateralis muscle is carefully elevated from the intermuscular septum and retracted anteriorly and medially, exposing the distal femur. Medial soft-tissue stripping should be avoided. In patients with intra-articular involvement, the initial step is reduction and stabilization of the condylar fragments (Fig. 28-48A). In cases in which the articular surface cannot be reduced anatomically, the tibial tubercle can be osteotomized to gain wide exposure of the condylar surfaces.232 Before the osteotomy the tubercle should be drilled and tapped. After adequate surgical exposure, the femoral condyles are reduced and provisionally fixed with Kirschner wires. Once reduction is confirmed, either clinically or radiographically, the condyles are definitively fixed with cancellous screws (see Fig. 28-48B). Washers are often indicated, depending on the quality of the bone stock. Placement of these cancellous screws should be anterior and posterior in the condyles, allowing sufficient space between them for subsequent insertion of the condylar blade plate or screw.
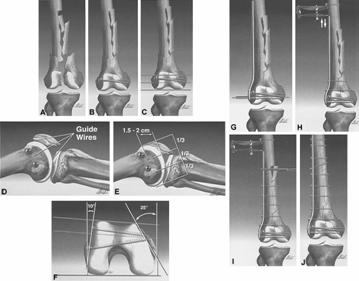
Fig. 28-48
The extra-articular supracondylar fracture is reduced next. In the simple fracture patterns, provisional Kirschner wire fixation or reduction with the aid of pointed reduction forceps will suffice. However, in comminuted fracture patterns reduction is best achieved with the aid of a femoral distractor. Placed directly into the femoral shaft proximally and anchored either in the distal femur or proximal tibia, distraction usually restores overall length and alignment. Initial overdistraction permits gentle teasing of comminuted fracture fragments into near-anatomical position. In comminuted supracondylar femoral fractures, it is often easier to reduce the fracture to the plate rather than the plate to the fracture. In this situation the plate may be used to aid reduction. Reduction is fine tuned with the aid of an articulated distraction-compression device. For proper positioning of a condylar blade plate or a dynamic condylar screw, orientation guide wires are necessary. The first guide wire is inserted parallel to the inclination of the anterior articular surface of the femur (patellofemoral joint). A second guide wire delineates the axis of the knee joint. The final guide wire is the definitive or summation guide wire and parallels the first two wires (see Fig. 28-48C and D) The correct starting point for the insertion of the seating chisel or triple reamer is in the anterior half of the femoral condylesin a line with the femoral shaft and exactly parallel to the summation guide wire. The starting point is 1.5 to 2.5 cm proximal to the articular margin of the knee joint (see Fig. 28-48E). In young patients with hard bone, insertion of the seating chisel may be difficult. To prevent iatrogenic comminution, a window should be created and predrilled to receive the seating chisel. Once the window is precut, the seating chisel is inserted to a predetermined distance. Remember that the distal femur is trapezoidal and the medial cortex slopes 25 to 30 (see Fig. 28-48F). When using either the condylar blade plate or screw, the tip of the implant should be 1 to 2 cm short of the medial femoral cortex to prevent inadvertent penetration (see Fig. 28-48G). Length and final alignment are enhanced with the femoral distractor or articular tension-compression device (see Fig. 28-48H). Once the plate has been inserted, the fracture should be placed under axial compression using the external tension device or by means of the self-compressing principle of the dynamic compression plate (DCP) (see Fig. 28-48I). However, only when the medial cortex is restored can the plate be effectively loaded. Properly done, the plate is placed under tension and is subject to load-sharing, rather than load-bearing (see Fig. 28-48J). In cases with significant comminution, the plate is fixed to the proximal and distal fracture, bypassing the zone of comminution. In this environment, the plate acts as an internal splint. However, the fracture fragments spanned by the plate are viable and capable of rapid consolidation if their soft-tissue attachments have been respected (Fig. 28-49).

Fig. 28-49 A) Fractura supracondilara deschisa tip IIIA C3 cu cominutie a distala a femurului.
B) Toaleta, drenajul si fixarea cu suruburi condilare dinamice. Nu s-a tentat reducerea anatomica. Ungimea si aliniamentul s-au realizat cu ajutorul unui distractor. C) La 9 luni exista un pod cortical de-a lungul corticalei interne si posterioare. Pacientul nu necesita sprijin extern.
When medial comminution or defects in the medial cortex exist, supplemental cancellous bone graft is necessary. Similarly, supracondylar fractures with extension proximally into the femoral diaphysis should probably be bone grafted. The most common donor site is the ipsilateral iliac crest. Alternative sites include the greater trochanter and proximal tibia. Bank bone or synthetic bone should only be used in closed fractures. In open, contaminated fractures these allograft materials are contraindicated.
Concomitant ligamentous injuries to the knee are uncommon and are rarely diagnosed preoperatively. Infrequently, bony avulsion injuries of the collateral or cruciate ligaments can be identified on the initial injury x-rays. Mid-substance tears and capsular disruptions cannot be assessed clinically owing to the close proximity to the fracture site. The most commonly injured ligament is the anterior cruciate. In supracondylar fractures with significant comminution of the articular surface the anterior cruciate ligament can be detached with one of the fracture fragments. Whenever possible this osteoarticular fragment should be repaired at the time of fixation of the supracondylar fracture.
There is no consensus regarding the timing of treatment of mid-substance tears of the cruciate ligaments associated with supracondylar fractures. Primary repairs, ligament augmentation, and formal reconstruction are made much more difficult by the presence of the fracture and associated internal fixation devices. Large caliber drill holes, or tunnels, made through the intercondylar notch of the femur for ligament reconstruction are usually contraindicated. They may cause further comminution of the fracture, compromise the stability of internal fixation, or be technically impossible because of the fixation hardware. Primary ligament repairs or reconstruction prolongs operating time and may increase the risk of postoperative infection, intra-articular adhesions, and loss of knee motion. Initial nonoperative treatment of mid-substance tears of the cruciate ligaments is recommended. Protected motion in conjunction with a knee orthosis together with vigorous rehabilitation may obviate the need for late reconstructive surgery in some patients. In those patients with persistent functional disability, late ligament reconstruction can be undertaken once the fracture has healed and the hardware can be removed safely.
There are two major types of internal fixation devices widely used in the management of supracondylar femoral fractures: condylar plates and screws and intramedullary nails. Because the spectrum of injuries to the supracondylar region of the femur is so great, no single implant will be suitable for every case. Careful assessment of the patient and critical review of the x-rays and the 'personality' of the fracture are essential. Some of the factors to be considered in this surgical decision-making process include (1) patient age, (2) the patient's ability to walk, (3) the degree of osteopenia, (4) the degree of comminution, (5) the condition of the soft tissues, (6) the presence or absence of open wounds, (7) involvement of the joint surfaces, and (8) whether the fracture is an isolated injury or one of many injuries.
In young patients, restoration of length and axial alignment with stable fixation and early functional rehabilitation remain the goal of surgery. In elderly osteoporotic patients, impaction of metaphyseal fragments with small amounts of shortening or malalignment may be a reasonable trade-off for rapid fracture union. Alternatively, Struhl and associates advocated the use of cemented internal fixation for supracondylar femur fractures in geriatric osteoporotic patients.254
95 Condylar Blade Plate For many supracondylar femoral fractures requiring operative stabilization, the 95 condylar blade plate remains a useful implant. There is a large body of literature in both North America and Europe documenting success with this method.210,216,217,244,249,251,252,262 When used by an experienced surgeon, this device restores alignment and provides stable internal fixation (Fig. 28-50). Because it is a one-piece device, it affords the best control of the fracture. However, placement of the 95 blade plate is a technically demanding procedure, because the surgeon is required to place the blade correctly in three planes simultaneously. This leaves little room for error in an already fractured bone. There is a moderately long learning curve associated with the use of this implant before consistent and reproducibly good results are achieved. It can be used in intraarticular fractures, providing the distal lateral femoral condyle is intact. In cases in which comminution extends distally and laterally compromising fixation, a condylar buttress plate is preferred. Use of the 95 blade plate in elderly patients with variable degrees of osteopenia must be individualized. Fixation or lag screws must have some purchase in all screw plate devices to be effective.
Dynamic Condylar Screw Several authors have reported favorable results in supracondylar femur fractures using a 95 compression screw and side plate.214,238,239,240,241,250 This device is based on the compression screw commonly used in hip fractures. The implant shares many of the features of a compression hip screw, making it familiar to most surgeons and therefore easier to master. Other advantages include its ability to apply interfragmentary compression across the femoral condyles, better purchase in osteoporotic bone, and the need for only two-plane alignment (see Fig. 28-49). By allowing a degree of freedom in the sagittal plane, insertion of this device is technically easier than a 95 blade plate. Should a nonunion develop after its use, the side plate can be replaced without revising the transcondylar screw. The major disadvantage with the dynamic condylar screw and plate is the bulky size of the implant at the screw-plate junction. This frequently requires removal of considerable bone from the lateral femoral condyle to ensure a low-profile fit. Despite modifications in its manufacture, the 'shoulder' of this device is more prominent than that of a comparable angled blade plate. In many patients this causes knee symptoms as the iliotibial band slides over the prominent edge of the implant. Additionally, the dynamic condylar screw and plate must be key-locked to prevent rotation within the barrel. In low supracondylar fractures, the condylar screw may not provide as much rotational control of the distal fragment as the 95 condylar blade plate. At least one additional screw placed through the plate and anchored in the distal fragment is necessary to ensure stable fixation.
Condylar Buttress Plate The condylar buttress plate is a one-piece device specifically designed for the lateral distal femur.221,222,231,234,242 It is essentially a broad dynamic compression plate with a cloverleaf-shaped distal portion designed to accommodate up to six cancellous screws (6.5 mm). Because the posterior portion of the cloverleaf is larger than its anterior counterpart, it is manufactured in left and right sides. Mechanically, the implant is not as strong as a blade plate or condylar screw and side plate, and therefore it should not be used or substituted for these preferred implants. The problem with the condylar buttress plate is that the screws passing through the distal holes do not have a fixed relationship to the plate. With indirect reduction techniques, if the plate is used in distraction or compression with the articulating tension device, the screws may shift relative to the plateproducing a varus deformity with distraction or a valgus deformity with compression.229 Use of this device should be restricted to cases in which the lateral femoral condyle is comminuted or there are multiple intra-articular fractures in the coronal or sagittal plane. In cases with extensive medial comminution a second medial plate is often indicated to prevent varus deformities (Fig. 28-51).242 When correctly inserted, the condylar buttress plate provides excellent alignment and stability (Fig. 28-52). It has also been used to salvage delayed unions and nonunions after use of a 95 blade plate or a dynamic condylar screw.
Reamed Intramedullary Nails Reamed antegrade intramedullary nails have a limited role in the management of supracondylar fractures. In diaphyseal fractures of the distal third of the femur an interlocking, intramedullary nail is probably the treatment of choice. However, in true supracondylar fractures, particularly those with intra-articular involvement and displacement, antegrade nailing is technically difficult and may not provide reliable fixation for many intra-articular fracture patterns. Nevertheless, Leung and associates226 reported the results of interlocking, intramedullary nailing for supracondylar and intracondylar fractures of the distal part of the femur in 37 patients (30 extra-articular and 7 intra-articular nailings). All fractures healed, and there were no malunions or infections. Functional outcome results were assessed with the modified knee rating system of the hospital for special surgery. There were 35% excellent, 59% good, and 5% fair results.
Perhaps the most common application for an antegrade, reamed, intramedullary nail is a fracture in the distal one third of the shaft with fracture extension into the supracondylar region or knee joint. Screw or plate fixation of the metaphysis and an antegrade nail provides an excellent method of treatment (Fig. 28-53).
Supracondylar Femoral Nail A retrograde intramedullary nail
designed specifically for supracondylar/intracondylar femur fractures has been
developed (Smith & Nephew Richards,
Potential disadvantages of the supracondylar nail include knee sepsis, stiffness, patellofemoral degeneration, and synovial metallosis resulting from nail or screw fretting or breakage.219
Lucas and associates227 reported the results of 34 supracondylar nailings in 33 patients. In short-term follow-up in 25 patients all fractures healed with an average arc of knee motion of 100. Four AO/ASIF type C fractures required bone grafts at 3 months; there was one bent and broken nail and one late infection with a septic knee. Six patients had arthroscopic or open lysis of adhesions for restricted range of motion of the knee. Iannacone and coworkers219 reported their experience with the supracondylar intramedullary nail in 38 patients with 41 fractures, which included 22 open and 19 closed injuries. There were four nonunions that required revision fixation and bone grafting. Two of five delayed unions required revision fixation. Thirty-five of the 41 knees achieved at least 90 of knee motion. There were no infections. Four patients developed fatigue failure of the implant, all of which occurred early in the series when 11- and 12-mm nails with 6.4-mm interlocking screws were used. There were no cases of implant breakage later in the series when the nail was modified to include 12- and 13-mm diameter nails and 5-mm locking screws.
Flexible and Semi-Rigid Nails Shelbourne and colleagues248 reported on the use of closed Rush pinning in 98 patients with supracondylar femoral fractures. Excellent and good results were obtained in 84% of patients, with only two nonunions and one deep infection. The nails provided enough stability at the fracture site to allow early knee motion. Several authors, however, have reported complications after Rush pin fixation of supracondylar femoral fractures. These have included pin migration, knee irritation, loss of reduction, and malunion. Routine use of these nails is not recommended.
In an attempt to overcome some of the pitfalls of Rush pinning, Kolmert and coworkers223 described the use of Ender nails connected to cancellous screws by a coupling device. This technique allows anatomical reduction of the femoral condyles using screws, as well as a semirigid connection of the condyles to the femoral shaft. Dynamic controlled motion at the fracture site occurs, which is thought to encourage healing. Most patients, however, require a cast or cast-brace for 8 weeks after surgery. I do not recommend this method.207
In 1970, Zickel and colleagues260 developed a nail specifically for use in the distal femur. The nail has a flexible stem and a rigid, curved condylar end allowing it to be anchored by transfixion screws into the femoral condyles. The Zickel nail was designed to be inserted by an open method, but closed nailing is possible. Fractures with intra-articular displacement require formal open reduction and a lag screw fixation before insertion of the Zickel device. Because the nail alone cannot prevent shortening in comminuted fracture patterns, cerclage wires are often necessary. Despite supplemental fixation, shortening can occur. Therefore, use of the Zickel nail should be restricted to noncomminuted or minimally comminuted supracondylar fractures in young patients and to elderly patients when impaction and shortening at the fracture site can be accepted.228 It is not recommended for fixation of corrective osteotomies in the distal femur; in such situations a plate with lag screw fixation across the osteotomy site and axial compression of the osteotomy is favored.
External fixation is used infrequently in supracondylar femoral fractures.247,253 The most common indication for its use is severe open fractures, particularly type IIIB injuries. In complex fracture patterns, supplemental lag screws are often necessary to fix intra-articular extensions. Depending on the location of the wounds and degree of fracture comminution, fixation across the knee is often necessary. For most patients the external fixator is a temporary device for initial management of the fracture and soft tissues. Once soft-tissue control is achieved, delayed internal fixation should be considered. Therefore, initial fixator pin placement should avoid areas of planned surgical incisions and implant placement whenever possible. As a general rule, 5.0-mm half-pins are inserted laterally above and below the fracture and connected to a unilateral half frame. If instability remains, a second plane of fixation is added, most often anteriorly with construction of a delta frame (Fig. 28-55).
Unlike tibial plateau fractures, ring fixators have a very limited role in the acute management of supracondylar femur fractures. Femoral frames tend to be large and bulky and frequently impede soft-tissue access in open fractures. Additionally, they require considerable time and expertise in application. These factors make ring fixators much less attractive in a seriously injured patient when time may be a critical factor.
The major indication for its use is an open supracondylar fracture with significant bone loss. Even in this circumstance, I favor conventional external fixation initially with application of the ring fixator as a reconstructive procedure when the patient's overall condition permits. Other indications for the use of a ring fixator are infected fractures and nonunions or malunions with combined deformities such as angulation, malrotation, or shortening. To minimize complications with the use of ring fixators, hybrid frames using small-diameter transfixing wires distally and half-pins proximally are recommended.
The major advantages of external fixation are rapid application, minimal soft-tissue dissection, the ability to maintain length, the provision of wound access, and the capability for mobilization of the patient. Problems associated with external fixation include pin track drainage and infection, loss of knee motion secondary to binding adhesions in the quadriceps mechanism, increased risk of delayed union or nonunion, and loss of reduction after removal of the device.
Occasionally, external fixation is recommended in the multiply injured patient with a closed supracondylar femoral fracture. When the patient's overall condition does not permit early definitive fixation, an external fixator can provide initial fracture stabilization until the patient can tolerate internal fixation.
The role for supplemental autogenous bone grafting has become less clear with the increased use of indirect reduction techniques and soft-tissue preservation methods. Whereas in the past comminution of the medial cortex was an absolute indication for bone grafting, current methods of fixation have eliminated the necessity for bone grafting in many complex supracondylar femur fractures. Strong indications for the use of bone grafts are fractures with bone loss or residual major bone defects. Relative indications include selected AO/ASIF A3, C2, and C3 fracture patterns, as well as many severe open fractures treated on a delayed basis to prevent nonunion. When grafting is necessary, I prefer autogenous iliac crest bone graft, except in osteoporotic elderly patients who invariably have little usable bone. In these cases, I use cancellous chips from a bone bank. Whenever possible, the bone graft is introduced through the fracture site in an area of comminution, minimizing additional soft-tissue dissection.
Author's Preferred Method of Treatment
Selecting a method of treatment for supracondylar femur fractures requires mature clinical judgment. The urge to operate must be tempered by a clear understanding of the benefits and risks. In elderly patients with stable impacted fractures, I prefer cast immobilization. Incomplete or nondisplaced fractures, regardless of age, rarely require internal fixation. Many extra-articular low-velocity gunshot wounds, particularly those that leave at least one cortex intact, are best treated without fixation. Similarly, severe osteopenia or neurologic impairment often dictates against surgical intervention. For most patients treated nonoperatively, early application of the cast-brace that allows knee motion is strongly recommended.
On the other hand, most displaced fractures in physiologically young patients should be stabilized surgically. For most fractures requiring fixation, my implant of first choice is a dynamic condylar screw and side plate. Correctly inserted, this device provides excellent fixation. It is particularly useful in supracondylar fractures with comminution extending proximally into the femoral shaft. Because it is a two-piece device, it allows a degree of freedom in the sagittal plane, thereby minimizing fixation errors. I prefer the 95 condylar blade plate for management of nonunions or to stabilize corrective osteotomies in the distal femur. When comminution involving the lateral femoral condyle is severe, I prefer the condylar buttress plate for fixation. If comminution on the medial side is extensive, bone graft with or without a medial plate is recommended strongly. Alternatively, a supracondylar interlocking nail may be used. If stable fixation has been achieved, postoperative CPM or early range-of-motion exercises should be instituted.
After irrigation and debridement of type I, II, and IIIA open supracondylar femur fractures, I believe the benefits of immediate internal fixation outweigh its risks. However, in type IIIB and IIIC open fractures with massive wounds, external fixation or delayed internal fixation is preferred. Repeated irrigation and debridement at 36- to 48-hour intervals until all devitalized tissue is removed is necessary to reduce the risk of infection. Once a clean wound has been achieved, internal fixation and bone grafting (if necessary) may be carried out.
|
Politica de confidentialitate | Termeni si conditii de utilizare |

Vizualizari: 3791
Importanta: ![]()
Termeni si conditii de utilizare | Contact
© SCRIGROUP 2025 . All rights reserved