| CATEGORII DOCUMENTE |
| Bulgara | Ceha slovaca | Croata | Engleza | Estona | Finlandeza | Franceza |
| Germana | Italiana | Letona | Lituaniana | Maghiara | Olandeza | Poloneza |
| Sarba | Slovena | Spaniola | Suedeza | Turca | Ucraineana |
In the last 20 years, the orthopaedic community has become more aggressive in operating on both isolated and combined cruciate ligament injuries. A nonoperative approach for isolated collateral ligament injuries, however, has been accepted for grade I and II sprains but remains controversial for grade III injuries (Fig. 29-83). The basis for these changes has been a better understanding of the biomechanical, histologic, and clinical studies of these injuries.
Although an earlier section of this chapter extensively detailed the ligamentous anatomy of the knee, a brief review of functional anatomy would be helpful before we discuss the pathology and treatment of ligamentous injuries.
On the medial side of the knee, three basic layers incorporate all the important stabilizing structures (see Fig. 29-84 and Fig. 29-9). Whether or not these structures are primary or secondary stabilizers, it is nave to discuss an injury to an isolated constituent of a layer. Typically, an injury to the MCL involves any or all of the structures from layers one to three. Layer one, the most superficial, is an investing fascia that from anterior to posterior encases the entire medial aspect of the knee and coalesces with the hamstring muscles and posteromedial capsule (see Fig. 29-9B). The second layer includes the superficial MCL, which has a very distal insertion on the medial aspect of the tibia at the level of the pes anserinus tendon. The deep MCL is the third or deepest layer of the medial structures (see Fig. 29-9D). Its posterior extension, the posteromedial capsule, includes the posterior oblique ligament described by Hughston.390,391,392,393,441
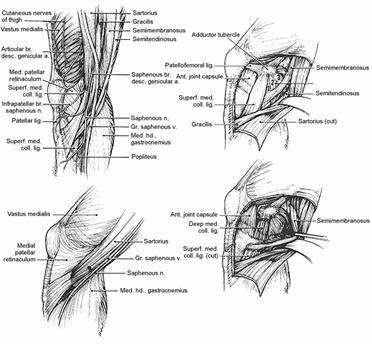
Fig. 29-9

Fig. 29-84 Relatia tibiei in diferite instabilitati rotational
On careful dissection, the posterior oblique ligament can be divided into three aspects: an inconsequential superficial fascial extension, a central portion that originates at the adductor tubercle and inserts on the posteromedial corner of the tibia, and a fascial covering that runs posteriorly and laterally, combining with one of the extensions of the semimembranosus tendon to become the oblique popliteal ligament (Fig. 29-85). The posteromedial corner also has an intimate relation with the semimembranosus tendon, and there may be a dynamic relation with this tendon and the posteromedial corner. Similarly, the origin of the superficial MCL is thought to be reinforced by a contribution from the vastus medialis obliquus. The medial capsular layers provide stability to valgus stresses at the knee; in fact, several authors have identified them as the primary stabilizer at 30 flexion.353,377,392,406,475
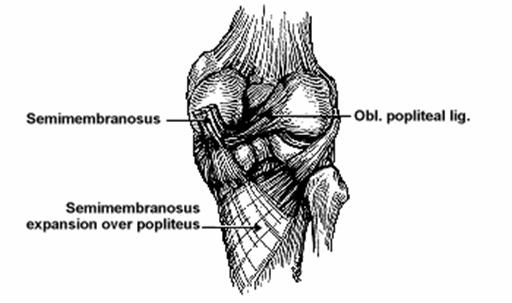
Fig. 29-85 Componentele ligamentului popliteal oblic
Selective cutting studies on cadavers have been conducted by Grood,377 Warren,475 and Inove396 and their colleagues. The MCL is the primary medial stabilizer at 30 flexion and a secondary contributor at full extension. In full extension, the ACL is a primary stabilizer, with a contribution from the posteromedial capsule.
In addition to these three layers on the lateral side of the knee (see Fig. 29-11), other anatomists, such as Kaplan,404 have described the quadruple complex as providing functional stability to varus stresses. This complex includes the iliotibial band, the biceps muscle and tendon, the LCL, and the popliteus. Another approach is to divide the lateral structure into three partsanterior, middle, and posterior thirds.388,393 The anterior third extends from the lateral border of the patellar tendon to the anterior border of the iliotibial band and includes the lateral retinaculum. The middle third includes the iliotibial band and its five layers, as described by Terry and colleagues.465 These five layers are the aponeurotic, superficial, middle, deep, and capsulo-osseous structures. The aponeurotic layer includes the fascia overlying the patella and patellar tendon; the superficial layer includes the vastus lateralis, iliopatellar band, lateral patellar ligament, iliotibial tract, and biceps femoris. The middle layer reinforces the superficial layer, whereas the deep layer begins 6 cm proximal to the lateral epicondyle, extends distally to the lateral femoral condyle, and inserts into the superficial layer. As its name suggests, the fifth layer, the capsulo-osseous layer, has a periosteal attachment and is reinforced by the short head of the biceps femoris.
The posterior third of the lateral supporting structures is known as the arcuate complex. It includes the lateral (fibular) collateral ligament, the arcuate ligament, and an extension of the popliteus muscle. The posterior third of the lateral ligamentous complex is reinforced by the biceps, popliteus, and lateral head of the gastrocnemius. The extracapsular fibular collateral ligament originates from the lateral epicondyle and attaches to the fibular head. In about 15% of patients, the short fibular collateral ligament is demarcated by the presence of a fabella confluent with the posterior aspect of the LCL. The arcuate ligament originating on the posterolateral aspect of the femur inserts distally onto the posterolateral aspect of the tibia and is reinforced by the biceps tendon. The posterolateral corner is also reinforced by the popliteus and the lateral head of the gastrocnemius muscles (see Fig. 29-11, Fig. 29-12 and Fig. 29-13).
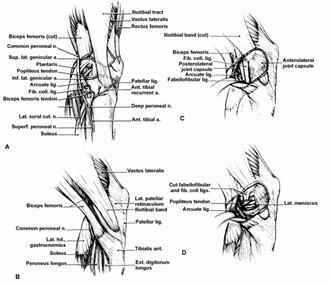
Fig. 29-11 A) Topografia structurilor laterale; B) Stratul unu include tractul iliotibial si portiunea superficiala a bicepsului femural; C) Stratul 2 include retinaculul lateral si ligamentele patelofemurale; D) Stratul 3 este capsula articulara si include ligamentele arcuat si fabelo-fibular.
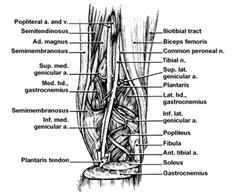
Fig. 29-12 Anatomia spatiului popliteu
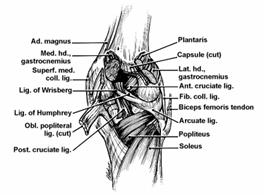
Fig. 29-13 Relatia ligamentului popliteu cu structurile musculare
Multiple experiments have been performed to assess the contribution of the lateral structures.404,411,444 According to Grood and associates,377 the LCL is a primary restraint to varus stress at both 5 and 25 flexion. The lateral capsule contributes to varus restraint, but only about a third that of the LCL from 0 to full extension and only half of that at 30 flexion. The anterior and middle thirds of the lateral capsule are a small, less significant secondary restraint to varus stress. The arcuate complex is similarly not very significant but provides twice the contribution of the anterior and middle thirds of the lateral capsule. This contribution, however, is diminished when the knee is flexed 25. The iliotibial band and popliteus tendon biomechanically play a very insignificant role in resisting varus stress statically; however, there is undoubtedly a significant dynamic stabilizing component.
Knee motion can best be described in terms of rotation, turning around an axis, and translation in three axes, the x, y, and z planes. The axes in the x, y, and z planes correspond to the motions of abduction/adduction, flexion/extension, and internal/external rotation. Translation, a slide along a particular axis, can be in either the anterior/posterior, medial/lateral, or proximal/distal directions. The ability of the knee either to rotate or to translate in the axes mentioned previously is called a degree of freedom. Natural knee motions do not occur with one degree of freedom, but rather several. Knee flexion, for instance, includes a rotation about a medial/lateral axis and translation along and rotation around an anterior/superior axis as well as a proximal/distal axis (personal communication, Minkoff, J., and Nicholas, J.A.).445 Coupled motions are two linked movements. For instance, in an anterior drawer test, the tibia translates anteriorly and rotates according to the pull of the examiner's left or right hand.
The joint is constrained by ligaments, tendons, the joint capsule, and the menisci. The primary and secondary constraint concept assigns each anatomic structure a level of importance based on its restraint within that degree of freedom. Sprains produce some elongation or rupture of either single or multiple collagen fibers. The Committee on Medical Aspects of Sports and the American Medical Association in their Handbook of Standard Nomenclature of Athletic Injuries classified injuries to these ligaments according to the number of fibers disrupted and the instabilities of the joints involved. A first-degree sprain is 'a tear of a minimum number of fibers (microtears) or less than one third' of a ligament. There is minimal hemorrhage and swelling, localized tenderness, and no clinical instability or laxity. A second-degree sprain is a tear of more ligamentous fibers (one third to two thirds) with a greater loss of function, localized tenderness, and an effusion, but there is no laxity or noticeable instability. A third-degree sprain implies more disruption (greater than two thirds), more tenderness, and demonstrable laxity of the knee joint (see Fig. 29-83).318
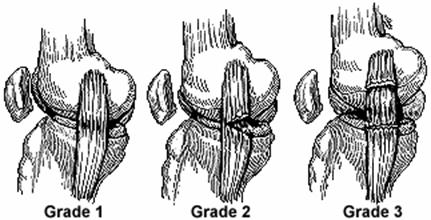
Fig. 29-83
Clinically, testing for a degree of injury is based on three grades, with grade 0 as normalthis implies that ligament testing from the injury to the contralateral leg shows no difference. Grade 1 (mild) is an opening of the joint of less than 0.5 cm. Grade 2 (moderate) is a 0.5- to 1-cm opening, and grade 3 (severe) is an opening greater than 1 cm.
Another method of classification of ligament instability has been advanced by the American Orthopedic Society of Sports Medicine's Research and Education Committee.319 Their classification is based on nonrotatory, or one-plane, and rotatory, or two-plane instabilities. One-plane instabilities, anterior/posterior, and medial/lateral are described in terms of 0 to 3+. Zero is normal, 1+ is a translation of 0.5 cm, 2+ is 0.5 to 1 cm, and 3+ is 1 to 1.5 cm. Throughout the literature, a grade 4 terminology has developed, representing a translation of greater than 1.5 cm.139,422 Rotatory instabilities include anteromedial, posteromedial, anterolateral, posterolateral, and combined (see Fig. 29-84). Although clinical tests for determining these instabilities are discussed later, they have specific meanings. Anteromedial rotatory instability implies tibial abduction, external rotation, and anterior tibial translation in which the medial tibial plateau translates or subluxates anterior to the femur. Similarly, anterolateral instability is an excess of anterior translation of the lateral tibial plateau. Posteromedial instability implies a posterior translation of the medial tibial plateau; posterolateral describes the abnormal posterior translation of the lateral tibial plateau.
Rotatory instabilities have similarly been classified from 0 to 3+. Combined instabilities, when present, can be of any combination. The most common are anterolateral/anteromedial, anterolateral/posterolateral, and anteromedial/posteromedial.444,445
Although many other attempts have been made to describe the instabilities in terms of the anatomic structure involved, these are not generally accepted and have as many shortcomings as the aforementioned prevailing classification system.
Mechanism of Injury
Collateral ligament injuries about the knee result from direct or rotational injuries. In an injury to the medial side of the knee, for instance, the force is almost always applied on the outside of the knee (Fig. 29-86). Similarly, an injury to the varus or lateral stabilizers of the knee occurs from an unopposed force applied to the medial side of the knee. The MCL may be more apt to be involved when the stress is in the straight lateral direction rather than rotational.422 The combination of a torsional and valgus mechanism of injury is more typical of an injury involving both the MCL and ACL.389,395,422 The magnitude of the valgus injury sequentially causes disruption of the primary medial stabilizer (the MCL) and possibly the secondary stabilizer (the ACL). These injuries are often but not always due to direct contact; noncontact injuries are common, especially in deceleration events in which the forces can be substantial.
Injuries of the lateral stabilizing ligaments of the knee result from a medially directed force, which almost always involves a rotational component applied to the tibia. Compared with valgus injuries, medially directed forces to the knee are uncommon. The involved lateral structures are the iliotibial band, popliteus tendon, LCL, and arcuate capsular complex. The cruciate ligaments can also be involved, once again depending on the magnitude of the force.
Ligamentous injuries are significant events, and the patient usually knows it (personal communication, Scott, W.N.).450 The patient with an isolated grade I or II injury might immediately return to a sporting event, but one with a grade III sprain rarely does so. A grade III sprain is typically associated with an ACL disruption. The patient often feels a ripping sensation and characteristically does not use the word 'pop' or give a 'two-fisted'454 sign, which is more typical of an isolated ACL injury. Tenderness is usually discrete and confined to the appropriate ligamentous complex. On the medial side, it can be anywhere along the course of the superficial collateral ligament (from the medial epicondyle 6 to 8 cm down the medial tibial shaft). LCL tenderness might be present anywhere from the lateral epicondyle to the fibular head. The patient will prefer some sort of protection, whether it be an Ace bandage, an immobilizer, or crutches, because the knee feels insecure with weight bearing.
On physical examination, point tenderness is in the area where the patient has felt the injury and is specific. It can almost always be duplicated on appropriate stressing of either the affected medial or lateral ligamentous complex. The degree of injury is manifested by the amount of opening, as discussed in the previous section. With an isolated collateral ligament injury, swelling is not always an absolute feature. If the capsule has not been disrupted, swelling is usually present and occurs within several hours, which suggests blood vessel disruption rather than a synovial reaction. A synovial reaction characteristically occurs with meniscal injuries in a delayed fashion (more than 6 to 8 hours). One should not feel comforted by an absence of swelling, however: this might indicate a significant injury that has disrupted the capsule. This disruption allows bleeding associated with ligament injury to dissect down the calf and thus is not apparent intra-articularly.
Collateral ligament testing is done in accordance with an understanding of the biomechanical function of each collateral ligamentous complex. On the medial side of the knee, the MCL, the primary stabilizer against valgus instability, is stressed at both 0 and 30 flexion. It is reinforced at 0 flexion by the secondary restraint, the ACL. At 30 flexion, the testing is specific for just the MCL. For a right knee, the examiner's left palm is placed at the lateral joint line, with the fingers going into the popliteal area. The palm of the right hand is placed against the medial malleolus, and the leg is gently manipulated with a valgus force by the examiner's right hand (Fig. 29-87). The left hand stabilizes the femur, and the resulting torque is resisted by the medial ligamentous complex. In addition to instability, pain is usually experienced by the patient, especially with grade I and II injuries.
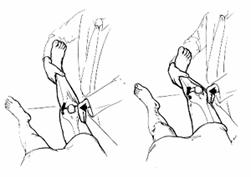
Fig. 29-87 Restarea lig. Colateral int. se face aplicand o forta de valg in extensie (pt. LIA Si LCI) sau 30 grade de flexie (pt. LIC)
Testing for lateral instability requires the reverse position of the hands. For the right knee, the examiner's right palm is placed on the medial aspect of the knee, the left palm over the lateral malleolus (Fig. 29-88). A varus force is gently applied through the examiner's left hand, with the patient experiencing discomfort (grades I, II, and III) and instability (grade II or III).
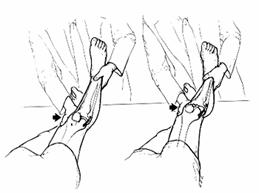
Fig. 29-88
Rotational tests are more indicative of combined collateral and cruciate ligament injuries and are discussed later.
Standard roentgenographic knee series do not reveal any injury to the collateral ligaments unless there has been a bony avulsion. In the chronic injury, however, it is common to see evidence of calcification at the origin of the MCL (Pellegrini-Stieda phenomenon).423 Stress films are helpful when more specific testing is unavailable (Fig. 29-89). Arthrography has been used to demonstrate leakage of dye, but it is inaccurate and depends on the timing of the procedure. If there is a complete disruption of the ligament, one can usually see an extravasation of dye at the site of the disruption (Fig. 29-90). This method is usually superfluous, however, if a good clinical examination is done. The potential advantage of an arthrogram is that it can delineate meniscal tears; the inaccuracy of arthrograms, however, and the advantages of MRI have made this arguably obsolete.458

Fig. 29-91 RMN in incidenta coronara. Sange si edem la nivelul tes. Subcutanat (sageata). Comparativ tractul iliotibial apare ca un semnal continuu inchis.
In addition to the previously discussed advantages of MRI in identifying meniscal lesions, it is helpful in delineating the site of disruption of the collateral complexes (Fig. 29-91 and Fig. 29-92). A collateral ligament tear is best visualized on T2 imaging as a high signal of edema and hemorrhage in the substance of the low-signal ligament. MRI also helps delineate grade II and III injuries in which ACL damage is suspected.
Arthroscopy easily demonstrates disruption of the capsular ligaments, but it is not as specific as MRI for delineating the superficial MCL. The primary role of arthroscopy in this situation is once again to determine absolutely the ACL status, as MRI is sometimes equivocal.
Isolated grade I and II collateral ligament injuries should be managed conservatively, provided the ACL has not also been disrupted. It is unusual for the ACL to be damaged with a grade I and II injury, but the physician must ascertain the status of the ACL before embarking on any treatment regimen.
The nonoperative approach consists of three phases: phase Ipain and inflammation control; phase IIstrengthening; and phase IIIreturn to functional levels.442 In phase I, pain is usually controlled by anti-inflammatory medication and ice massage. Rarely, a very painful injury cannot be controlled by these maneuvers. Immobilization, which is done for symptomatic reasons, can be discontinued within 5 days. Quadriceps-strengthening exercises should be started and can be done by the patient or with the help of a physical therapist. The patient should avoid quadriceps-setting exercises in hyperextension, as they accentuate patellofemoral symptoms. Protection in the form of a cane or sleeve brace is recommended for the first week. In phase II, the strengthening program is intensified. Several programs have been recommended, including those of Steadman462 and Shelbourne and Nitz.451 A sleeve-type brace with a hinge should be used throughout phases I and II and even in phase III, which is a return to more functional activities such as running and cutting. The patient is returned to his or her environment, slowly progressing to running activities while continuing strengthening. It is important not to begin phase III until there are no symptoms of discomfort, either on direct palpation or on varus or valgus stress test to the appropriately injured collateral structure.
In grade III collateral ligament injuries in which the ACL and PCL are not involved, nonoperative treatment is also preferred. Although there are some proponents of operative intervention,436 several studies have shown conservative treatment to be superior to operative intervention.361,380,462 Indelicato395 performed a prospective comparison of operative versus nonoperative treatment and showed that patients in the nonoperative group returned to their sports 3 weeks earlier and had no significant long-term knee dysfunction or instability. Conversely, a report by Kannus403 showed poor results in a 9-year follow-up of grade III MCL injuries treated nonoperatively.
In summary, the patient should be treated initially to reduce discomfort while protecting against reinjury with walking aids, crutches, or a cane and a ligamentous sleeve brace. Once discomfort is minimized, strengthening is progressed until parity is realized. Progression to sporting activity is begun only after there is parity of strength and clinical tests for tenderness and instability are negative. A more detailed approach to the nonoperative rehabilitation of this injury has recently been presented by Saraniti and associates.449
Operative Treatment
Operative treatment of collateral ligament injuries is usually confined to combined cruciate and collateral ligament injuries. In isolated grade III injuries, most surgeons prefer a nonoperative approach. Surgically, a direct end-to-end suture is permissible, but an interlacing Bunnell-type repair is more advisable. Stiffness can be a major problem in collateral ligament repair, and thus the repair should not be too tight and should be reattached anatomically (Fig. 29-93). The issue of treatment with combined injuries is discussed separately. MCL injuries can be approached through a direct medial incision over the collateral structure, preferably localized to the area of maximum tenderness and disruption (Fig. 29-94). If surgical repair is deemed necessary, a preoperative MRI is advisable to determine the extent of the MCL or LCL injury. Similarly, in tears of the MCL and posterior oblique ligament, Hughston advocates careful dissection or reattachment of the posterior oblique ligament (Fig. 29-95). Hughston advocates repair of the medial ligaments, as this eliminates anteromedial rotatory instability.386 Other procedures for collateral instability have included the pes anserinus transfer (Fig. 29-96) for medial instability. For lateral instability, the more popular procedures include the Losee 'sling and reef' technique for lateral extra-articular instability (Fig. 29-97 and Fig. 29-98), the Andrews lateral tenodesis of the iliotibial band (Fig. 29-99), the Hey-Groves fascia lata technique (Fig. 29-100), and a proximal en bloc advancement of the popliteus tendon, LCL, arcuate ligament, and lateral head of the gastrocnemius (Fig. 29-101). Allograft reconstruction of the LCL (Fig. 29-102A and B) and the posterolateral corner (Fig. 29-103) have been popularized.328,329
Authors' Preferred Method of Treatment
In isolated collateral ligament injuries, there is no reason to operate. The major issue is to establish the integrity of the cruciate ligaments and meniscus. If neither the ACL nor the PCL is involved with the collateral ligament injury, the treatment should be nonoperative as outlined previously. (Meniscal lesions are tested arthroscopically.) Most patients with isolated grades I to III ligament injuries can return to a full sporting life in 6 to 12 weeks. The less severe the injury, the quicker the return. Patients prefer to use a hinged knee brace for some time while returning to sports, so we keep them in this type of brace for about 6 months after the injury, at which time stability is reassessed.

Fig. 29-94 Sutura capsulei se poate face cu fire separate sau intrerupte.
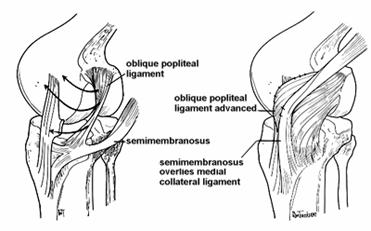
Fig. 29-95 Avansarea lig. Oblic posterior (Houghston)
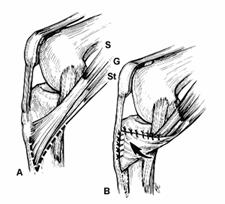
Fig. 29-96 Transferul pes anserinus in instabilitatea anterioara si anteromediala

Fig. 29-97 Tehnica sling and reef in instabilitatea laterala extraarticulara
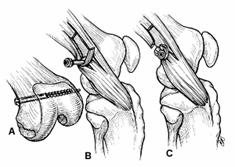
Fig. 29-99 Tenodeza laterala Andrews a tractului iliotibial
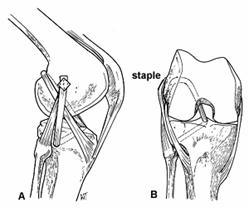
Fig. 29-100 Tehnica Hey-

Fig. 29-101 Tehnica de avansare in bloc a tend popliteu, LCE, lig. Arcuat si capul lateral al gastrocnemianului.
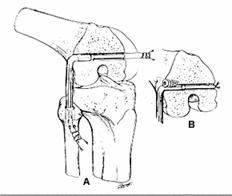
Fig. 29-102 Reconstructia LCE folosind alogrefa BTB. A)Fixarea grefei cu o sututra peste un pod osos; B)Fixarea cu surub de interferenta.

Fig. 29-103 Reconstructia LCE si tendonul popliteu folosind o grefa divizata BTB
Complications
When treated conservatively, isolated injuries to the collateral ligaments are usually not associated with future instability or meniscal lesions. Indeed, meniscal lesions are rareless than 4% of the time with grades I and II injuries and 0% to 13% with grade III injuries.353,414,442,444 Thus, it is important not to overtreat these injuries: surgeons should avoid an operative approach when nonoperative treatment protocols have had universally good success.
|
Politica de confidentialitate | Termeni si conditii de utilizare |

Vizualizari: 5976
Importanta: ![]()
Termeni si conditii de utilizare | Contact
© SCRIGROUP 2024 . All rights reserved